Suboxone (buprenorphine/naloxone) is the gold standard medication for opioid use disorder (MOUD) treatment—but it’s important to understand all of Suboxone’s pros and cons because it’s not the best choice for every person. Here is a guide on the pros and cons of Suboxone to help you have an informed discussion with your medical provider about which MOUD treatment is right for you.
Is Suboxone the best therapy for OUD?
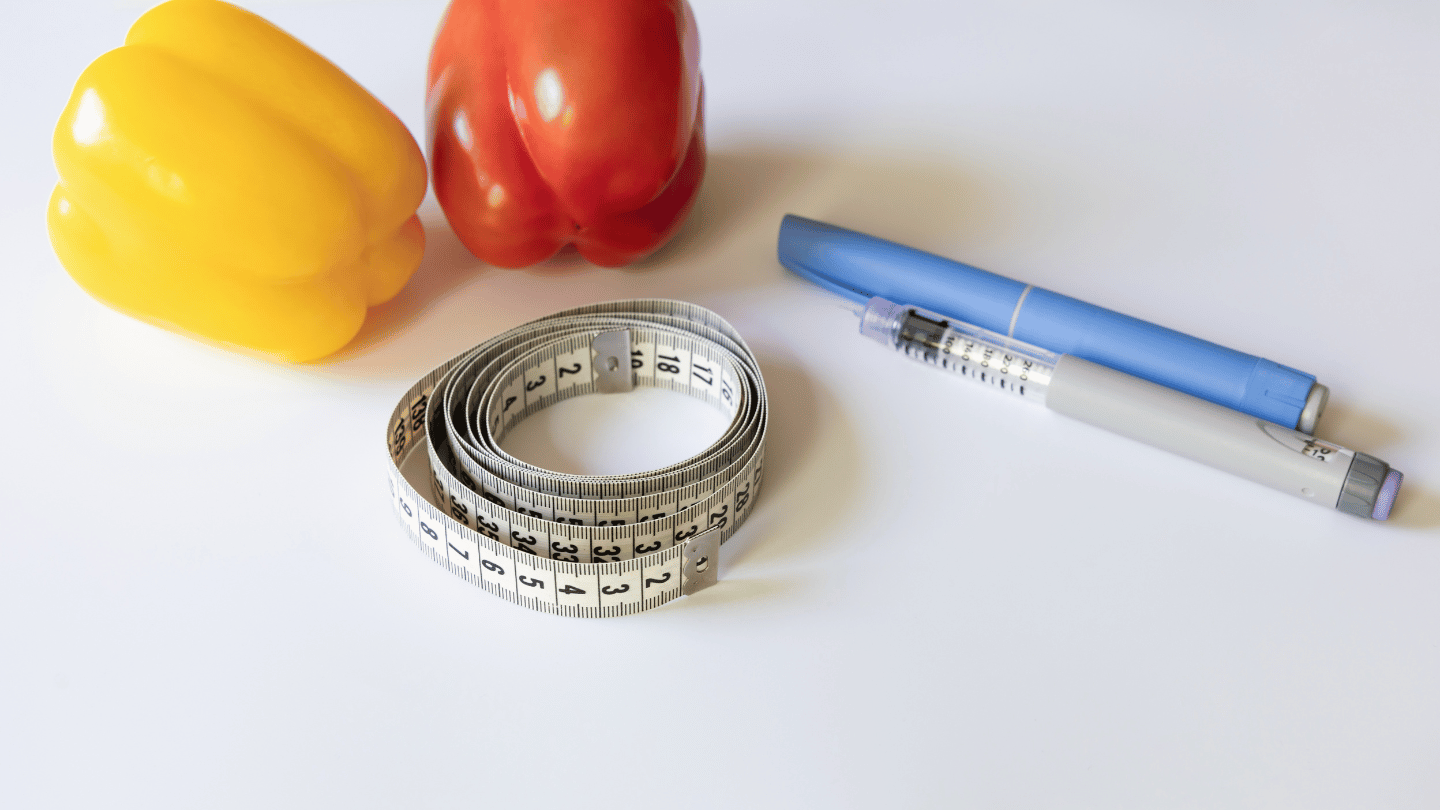
Suboxone (buprenorphine-naloxone) is one of several opioid addiction treatment options—and its active drug, buprenorphine, is one of just three medications approved for treating OUD (the other two being methadone and naltrexone).
To fully understand the benefits of taking Suboxone, you must compare it to all of the possible alternatives:
- Taking prescribed methadone
- Taking prescribed naltrexone
- Medically supervised withdrawal (detox) followed by abstinence
- Going cold turkey on your own (never recommended)
- Self-medicating with opioids/continuing opioid misuse (never recommended)
When you weigh the pros and cons of all these options, Suboxone usually comes out on top. That’s partly because even the cons of Suboxone are not “deal breakers” for most people with opioid use disorder (OUD).
So let’s start with the cons.
Suboxone con #1: The possible side effects
The most common side effects of taking Suboxone are constipation, nausea, vomiting, insomnia, pain, increased sweating, and headache. Other less common side effects have also been reported, such as fatigue, dizziness, tooth decay, muscle cramps or tremors, fast heartbeat, and attention problems. The rates of these side effects, however, are lower with Suboxone compared to methadone.
Some of these symptoms can be successfully treated with other medications or lifestyle changes, such as eating more fiber, drinking more water, and getting more sleep and regular exercise. Another strategy is to take lower doses of the medications more frequently throughout the day. For example, taking 4 mg of buprenorphine twice per day instead of 8 mg once per day. Your provider will recommend the best treatment plan for you.
In rare cases, side effects can be caused by the naloxone component of the Suboxone. If this is the case, buprenorphine by itself (sometimes called Subutex) can be prescribed.
Suboxone con #2: The withdrawal when starting
The traditional method of starting Suboxone can be rough because you must first go into moderate opioid withdrawal before you can take your first dose of Suboxone.
But, while this sounds awful, non-opioid drugs can be prescribed prior to starting Suboxone to help relieve the withdrawal symptoms you’re having.
Suboxone con #3: The withdrawal when stopping
Anytime someone with OUD or opioid dependency suddenly stops taking an opioid, withdrawal symptoms are bound to follow. This goes for all opioids—including prescribed Suboxone and methadone. Slowly reducing your dose (tapering off) of Suboxone with the help of a medical provider is the most effective way to stop taking Suboxone.
If you stop taking Suboxone without tapering you are likely to develop opioid withdrawal. Severe withdrawals can cause relapse in recovery and lead to overdose, which can be deadly.
Overcoming the cons of Suboxone
As you can see from the list of cons, the downsides of Suboxone mostly center around how your body physically reacts to buprenorphine.
Fortunately, most people who experience side effects with Suboxone are able to accept or overcome them and enjoy the benefits of recovery.
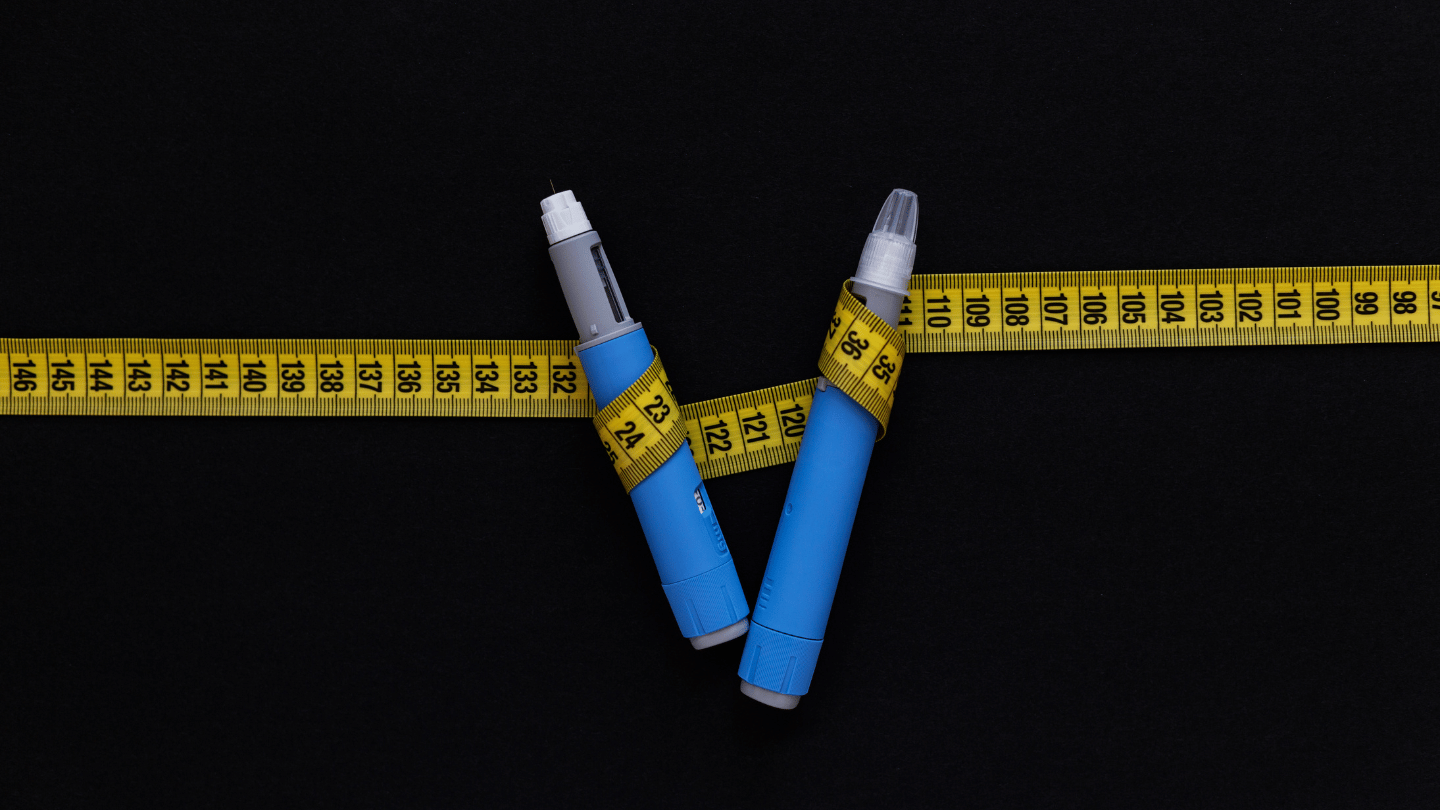
Suboxone pro #1: Cravings eliminated—or at least reduced
Suboxone attaches to the same opioid receptors that prescribed and non-prescribed opioids do—but Suboxone interacts with those receptors in a different way. As a result, Suboxone can take away your cravings without getting you high, helping you stop the cycle of opioid misuse and withdrawals.
Suboxone pro #2: Lower risk of misuse and relapse
Compared to other opioids, Suboxone has a lower risk of misuse. This is due to the unique effects of Suboxone compared to every other opioid available. Its effects on the brain and at the cellular level are different compared to all other opioids, which greatly lowers its risk for misuse.
If you quit opioids completely—even if you taper off of them slowly—your risk of returning to opioid use (relapse) is unfortunately very high. That’s because after withdrawal or detox is complete, you will likely continue facing strong cravings for opioids. Suboxone can prevent relapse by controlling cravings and helping you continue to say no to opioid misuse.
Can you overdose on Suboxone?
There are very few cases of people overdosing on Suboxone.
The real threat of overdose comes when you stop taking Suboxone and start using a full-agonist opioid such as Vicodin, codeine, Oxycontin, heroin, fentanyl, etc.
While you are taking buprenorphine as directed, the medication protects you from overdose and intoxication—but if you stop taking your Suboxone and start taking full-agonist opioids again, it’s very easy to overdose.
Suboxone pro #3: Cost and insurance coverage
As with most medications, the brand-name version of Suboxone is more expensive than the non-branded (generic) forms. For 1 brand-name Suboxone film with 8 mg of buprenorphine (and 2 mg of naloxone), the retail price is roughly $9.50, and only about $2.50 for the generic version. Based on pricing listed on the GoodRx website, the tablets tend to cost less than the films.
Fortunately, most insurance providers, including Medicaid in most states, cover the cost of generic Suboxone (buprenorphine-naloxone) for OUD.
To compare prices at pharmacies in your area, visit the GoodRx Suboxone Film page and the Generic Suboxone Filmpage.
Suboxone bonus benefit #1: Medication access via telehealth
With Suboxone, there’s no need to drive to a clinic or doctor’s office to get your meds (as you generally must do to receive methadone or naltrexone). The federal government has recognized that increasing access to Suboxone is a good thing—and as a result, they allow telehealth providers who are registered with the DEA to prescribe Suboxone to patients who need it through an online virtual visit, with generally no need for an in-person consultation. There are a handful of states that do require an in-person consultation at least once a year, to continue receiving treatment via telemedicine.
Suboxone bonus benefit #2: Ongoing research to improve Suboxone care
Millions of people have sought recovery from opioid use disorder, and continue to do so—and it’s encouraging to know that doctors and researchers are always learning new ways to improve treatment with Suboxone.
Here are just a few examples of how Suboxone treatment continues to improve over time:
- Opioid treatment providers are pushing for better access to Suboxone—and the federal government is listening
- Researchers and medical providers continue finding better ways of starting patients on Suboxone
- Opioid treatment specialists are re-evaluating Suboxone doses for those addicted to potent opioids like fentanyl
Suboxone bonus benefit #3: Relief from pain
People with opioid use disorder who also suffer from pain find that Suboxone can treat both. Even compared to other pain relief medications, buprenorphine has been proven to be an excellent drug for pain relief. However, telehealth prescribing of buprenorphine for pain alone is not a legal practice. Prescribing buprenorphine for patients with opioid use disorder or dependency AND pain, though, is acceptable.
Ready to start MOUD treatment with Suboxone?
QuickMD can answer your questions about Suboxone’s pros and cons, provide counseling for opioid use disorder, and send a prescription for Suboxone or generic buprenorphine/naloxone to the pharmacy of your choice the same day as your appointment. Contact QuickMD today to start online treatment for OUD in the comfort of your home.